
Referential and Reviewed International Scientific-Analytical Journal of Ivane Javakhishvili Tbilisi State University, Faculty of Economics and Business

Strategies for Overcoming Barriers to the Integration of Artificial Intelligence (AI) in Pharmaceutical Practice in Georgia
doi.org/10.52340/eab.2025.17.02.04
The integration of Artificial Intelligence (AI) into the pharmaceutical sector has the potential to significantly enhance healthcare services. However, several challenges hinder its effective adoption. This study examines the key obstacles facing Georgia’s pharmaceutical industry, including technological, regulatory, educational, and infrastructural barriers. Through a literature-based approach, the paper explores strategies to overcome these challenges. Key findings emphasize the necessity of modernizing pharmacy education, increasing investment in research and development, and strengthening collaborations between the public and private sectors. Additionally, addressing data privacy concerns and rising public awareness are essential for fostering trust in AI technologies. The discussion underscores the importance of aligning local regulations with international standards and promoting continuous professional development. Ultimately, overcoming these challenges will enable Georgia to successfully implement AI, leading to improvements in the quality, efficiency, and ethical standards of pharmaceutical services while ensuring patient safety.
Keywords: Artificial intelligence, innovative technologies, barrier, pharmaceutical practice, digital transformation.
JEL Codes: I10, I18, O33, L65, K32, I23, D83
Introduction
The adoption of innovative technologies, particularly artificial intelligence, is transforming pharmaceutical practice by introducing advanced tools to improving patient care, optimize medication management, and support evidence-based decision-making. AI has the potential to enhance clinical accuracy, minimize human error, and boost the overall efficiency of pharmaceutical services. In many parts of the world, these technologies are becoming integral to healthcare delivery systems, helping both practitioners and patients achieve better outcomes.
However, successful integration of AI into real-world practice requires more than technological readiness. It necessitates comprehensive structural changes, including the establishment of robust regulatory frameworks, the modernization of educational programs, and sustained collaboration among industry, academia, and policymakers. In Georgia, where the pharmaceutical sector is evolving, AI presents a promising opportunity for service modernization and improved healthcare quality. Yet, this process is hindered by several systemic challenges, such as limited digital infrastructure, insufficient workforce training, and outdated regulatory mechanisms.
Overcoming these obstacles is crucial to ensuring the ethical, effective, and sustainable application of AI within the Georgian pharmaceutical context. This study examines these challenges and presents strategic solutions tailored to the country’s healthcare environment.
Research Objective
The aim of this paper is to analyze the significance of artificial intelligence in pharmaceutical practice, explore the barriers to its integration in Georgia, and propose strategies for overcoming these barriers. Additionally, the paper seeks to provide recommendations for the successful adoption of AI, helping Georgia’s pharmaceutical sector leverage in Georgia in effectively and innovativetechnologies to enhance patient care and optimize service efficiency.
Methodology
This research employs a qualitative approach to examine the key challenges that hinder the integration of artificial intelligence into pharmaceutical practice in Georgia and at formulating practical strategies to overcome them. The methodological approach is structured around two main objectives: first, to identify the significant barriers to AI adoption - such as limited financial resources, data protection concerns, and security issues, and gaps in technical infrastructure - and second to develop feasible and ethically grounded recommendations for the sustainable and efficient application of AI within Georgia’s pharmaceutical sector.
To achieve these objectives, the study employs two interconnected methodological strategies:
1. Literature Analysis: A comprehensive review of scholarly articles, policy frameworks, and industry reports was conducted to assess global and regional trends in the integration of AI into pharmaceutical systems. Particular attention was given to case studies paid to evidence from countries with similar socio-economic profiles, as well as successful AI adoption in advanced healthcare settings. This body of literature serves as both a conceptual foundation and an empirical reference for identifying common barriers and drawing parallels with Georgia’s unique context.
2. Critical Examination of Primary and Secondary Materials: In addition to academic literature, the study evaluated a range of sources, including official documents, expert analyses and industry reports. These materials were critically assessed to build a comprehensive understanding of the challenges facing AI integration and to evaluate the readiness of Georgia’s pharmaceutical sector for AI-driven innovation. The inclusion of diverse information sources enabled triangulation, enhancing the reliability and applicability of the study’s findings.
The methodological framework ensures a well-rounded and in-depth exploration of the research topic, allowing for the development of context-sensitive, actionable recommendations tailored to the specific needs and conditions of Georgia’s pharmaceutical practice.
Results
Artificial intelligence is playing an increasingly transformative role in pharmaceutical practice, particularly in supply chain optimization, operational efficiency, and rapid response capabilities. Through predictive analytics and machine learning, organizations can anticipate supply needs, regulate inventory more effectively, and swiftly manage logistical disruptions—an essential function given the complexity of pharmaceutical distribution (Abd-alrazaq et al., 2022).
Among AI’s most impactful contributions is its precision in demand forecasting. By enabling pharmaceutical companies to allocate resources more strategically, AI helps minimize overstock or shortages, ensuring better medication availability. This, in turn, enhances patient satisfaction and reduces operational waste (Amosu et al., 2024; Sharma & Verma, 2023).
In addition, AI enables more precise inventory control by continuously analyzing usage patterns and stock flow, helping to maintain optimal inventory levels. This approach not only reduces costs but also ensures compliance with regulatory requirements, fostering lean and sustainable supply chains (Riad et al., 2024). AI’s ability to monitor supply chains in real time enhances resilience by automatically identifying and responding to disruptions. By increasing supply chain visibility and reducing human error, AI supports more stable pharmaceutical operations (Kampanart Huanbutta et al., 2024). AI's also plays a critical role in pharmacovigilance, enabling real-time safety monitoring after drug approval. By analyzing clinical and digital sources—including social media—AI helps detect adverse drug reactions early, facilitating preventive measures and strengthening public health safeguards (Kumar, Thakur, & Rana, 2022).
Within pharmacies, AI automates dispensing systems, improving speed and accuracy while minimizing errors. Smart technologies enhance medication adherence, enable real-time health monitoring, and assist in developing individualized treatment plans. AI-powered apps and wearables further promote health literacy and empower patients in self-care. Additionally, pharmacists benefit from tools that analyze drug interactions and support clinical decisions, cultimately leading to better patient outcomes and improved workflow efficiency (Noorbakhsh-Sabet et al., 2019).
This technological shift strengthens the pharmacist’s role in delivering patient-centered care. AI enhances safety and effectiveness, and its integration is transforming the healthcare landscape, creating new opportunities for innovation and collaboration (Zhang, 2023). Additionally, AI aids in patient education by simplifying instructions, promoting healthier lifestyles through digital engagement, and supporting remote monitoring via connected devices. Together, these advancements foster stronger communication between patients and healthcare providers (Saha Aritra et al., 2021).
AI is already revolutionizing key areas such as diagnostics, treatment design, drug development, personalized medicine, and patient surveillance. Pharmacies are evolving from traditional drug dispensers to proactive healthcare providers, offering immunizations, chronic illness support, and health tracking. with AI-powered tools enhance their ability to monitor and assist at-risk populations (Topol, 2019).
Healthcare professionals are using AI to choose optimal therapies, analyze clinical data, and accelerate decision-making – helping conserve resources and potentially saves lives (Wang, Kung, & Byrd, 2020). This progress is driven by improvements in data accessibility, computing power, and machine learning techniques. Across various medical fields, from oncology to hospital medicine, AI enables clinicians to tailor treatments to individual patient profiles, reduce diagnostic errors, and enhance the design of clinical trials (Liu et al., 2020). In today’s pharmaceutical landscape, AI-powere systems are increasingly used to assess and identify medication-related risks. As these technologies evolve, pharmacists will play a more advisory and preventive role, utilizing data to enhance patient engagement and promote health. (Yin et al., 2021; Shashiashvili., 2025).
Ultimately, AI empowers pharmacists to make data-driven decisions, integrating medical histories, laboratory results, and drug profiles to support personalized pharmacotherapy. By mitigating adverse interactions and side effects, AI contributes to safer and more effective treatment outcomes (Sharma & Verma, 2023).
Although artificial intelligence (AI) holds the potential to revolutionize healthcare systems, its effective implementation is hindered by a range of complex and interrelated challenges. One primary technical obstacle involves the quality and structure of available medical data. Clinical records sourced from healthcare institutions are often incomplete, inconsistent, or poorly formatted, which weakens the accuracy of data-driven insights. These limitations compromise the performance of advanced AI models, including neural networks, decision trees, and Bayesian inference systems. Additionally, mismatches between algorithmic design and specific data types can reduce the reliability of AI-driven clinical decision support tools (Wiljer et al., 2019).
Another critical challenge is the lack of robust clinical evidence supporting AI interventions. Many AI models are developed and tested within controlled environments or retrospective analyses, restricting their applicability to real-word medical practice. This gap between experimental results and practical implementation complicates integration efforts. Furthermore, uncertainty surrounding liability presents a legal and ethical dilemma—when AI-driven recommendations lead to medical errors, it remains unclear whether responsibility lies with the healthcare provider using the system or the developers who created it (Sengupta et al., 2024).
Social concerns also play a significant role in the adoption of AI in healthcare, particularly the fear that intelligent systems may displace human professionals. This perception can lead to hesitancy among staff. Addressing these concerns requires a robust training infrastructure to equip healthcare providers with the skills necessary for safe and effective use of digital technologies. At the same time, the introduction of AI must be supported by well-defined regulations that govern its use, protect patient data, and uphold ethical standards (Hofweber & Walker, 2024).
The integration of AI tools – particularly generative models – also presents notable regulatory challenges. These systems may inadvertently collect, store, or analyze sensitive information without obtaining adequate legal consent, potentially violating privacy laws. Ensuring compliance with data governance standards and secure handling protocols is essential to mitigate such risks (Mosley et al., 2024).
For AI to function reliably within real-world healthcare settings, its adoption must be based on rigorous clinical validation and supported by an evidence-based framework. At he same time, ethical guidelines and digital literacy among healthcare professionals must evolve in parallel. AI should be seen not as a replacement for human expertise, but as an advanced augmentation tool that enhances decision-making and improves patient outcomes.
AI systems hold significant promise for enhancing operational accuracy, reducing workload, and improving professional satisfaction in the pharmaceutical sector. However, the realization of these benefits requires overcoming several persistent implementation challenges:
1. Privacy and Security: The handling of personal medical data demands stringent safeguards, including robust encryption and clear mechanisms for informed consent. The controversy surrounding the UK's National Health Service and DeepMind highlighted the ethical pitfalls of sharing health data without explicit patient approval. To maintain public trust, AI-driven healthcare system must adhere to the highest standards of security and transparency. Additionally, ethical dilemmas may arise if patients reject AI-generated treatment recommendations, underscoring the importance of preserving autonomy and respecting individual preferences (Agarwal & Gao, 2024).
2. Physician Readiness and Acceptance: One of the major barriers to AI adoption is the readiness of physicians to engage with these technologies. Studies indicate that over half (62.4%) of clinicians feel inadequately prepared to work with AI, raising concerns about communication breakdowns and diminished trust in the physician-patient relationship. To ensure meaningful adoption, promoting technological fluency through continuous education and involving healthcare professionals in system development processes is essential. (Bryan & Li, 2024).
3. Algorithmic Bias: AI tools trained on datasets that lack demographic diversity risk perpetuating systemic inequalities. When training data fails to adequately represent all population segments, algorithms may produce suboptimal or even harmful recommendations for underrepresented groups, exacerbating healthcare disparities and compromising the fairness of clinical decision-making (Norori et al., 2021).
4. Automation Errors: Flawed training datasets or incomplete clinical inputs can result in incorrect AI predictions, posing serious safety risks. Errors in drug selection, dosage recommendations, or contraindications may lead to adverse medical events. A notable example is IBM’s Watson for Oncology, which faced criticism for generating inappropriate treatment options due to inconsistently curated training data (Hofweber & Walker, 2024).
5. Data Complexity and Accessibility: Medical data varies widely in type and format, including free-text notes, diagnostic images, lab results, and patient monitoring videos. AI tools require vast amounts of well-structured, harmonized data to function effectively. When data is fragmented or poorly standardized, AI predictions lose accuracy and practical utility (Sengupta et al., 2024).
6. Ethical and Equity Concerns: The use of AI in healthcare presents critical ethical challenges related to transparency, justice, and privacy. Biases embedded in training data may lead to discriminatory outcomes, while inadequate patient awareness about AI-driven processes can weaken trust. Ensuring patients have meaningful control over their personal data and a clear understanding of its use is essential for fostering ethical AI adoption (Agarwal & Gao, 2024).
7. Technical Challenges: A key obstacle to AI integration in healthcare systems is the issue of data standardization. AI requires high-quality, consistent, and diverse datasets for effective model training. However, medical data often lacks uniformity or exists in unstructured formats, diminishing the accuracy and reliability of AI-driven predictions (Mosley et al., 2024). Interoperability with clinical systems further complicates adoption. Healthcare providers utilize different data formats, making it difficult to integrate AI smoothly into existing infrastructures, which in turn hinders widespread implementation (Bryan & Li, 2024). Another significant limitation of many AI models is their lack of transparency and validation. Many function as "black boxes," generating decisions without clear explanations. This opacity weakens trust in AI-driven healthcare solutions, underscoring the need for rigorous validation protocols to ensure their reliability (Hofweber & Walker, 2024). Additionally, financial constraints pose a considerable challenge. Developing, deploying, and maintaining AI technologies requires significant financial investment, which can be particularly prohibitive in resource-limited settings where funding is already restricted.
8. Operational Challenges: For AI systems to be truly effective, they must be fully integrated into clinical workflows, complementing the work of healthcare professionals and ensuring alignment with daily operations. Without proper integration, AI systems risk being underutilized or failing to provide meaningful support in clinical practice. The engagement of key stakeholders, including physicians, patients, and regulatory bodies, is essential for successful AI adoption. The trust and cooperation are critical to sustaining AI technologies in healthcare (Sengupta et al., 2024). However, the rapid pace of technological development presents another challenge. AI technologies evolve quickly, while regulatory frameworks often lag behind, making it difficult to establish clear, adaptable standards for the safe and consistent implementation of new technologies (Mosley et al., 2024). Safety and efficacy are also pressing concerns. Despite AI’s potential to revolutionize healthcare, there is a risk of incorrect or biased recommendations, patient misclassification, and overlooked diagnoses. To mitigate these risks, rigorous preclinical and clinical is necessary to verify AI system reliability before widespread adoption (Bryan & Li, 2024). Furthermore, the lack of global harmonization in regulatory standards creates barriers to the international implementation of AI. Variations in regulations across countries can increase costs and hinder collaboration, preventing the establishment of uniform global standards (Agarwal & Gao, 2024).
9. Specific Challenges: AI offers promising solutions in the fight against antimicrobial resistance (AMR) by optimizing treatment pathways using patient-specific data, supporting antibiotic discovery, and predicting resistance trends. Additionally, AI can help prevent the spread of infections and improve treatment strategies. However, several challenges must be addressed:
• Limited or inconsistent datasets hinder the accurate training of AI models, which affects the system's ability to provide reliable predictions.
• Algorithmic bias is a concern when AI models are trained on non-representative datasets, potentially leading to unreliable results.
• Integration difficulties with existing digital health systems can reduce the effectiveness of AI in improving healthcare outcomes (Norori et al., 2021).
10. Public and Human Factors: The successful implementation of AI in healthcare relies heavily on the trust and acceptance of both physicians and patients. Concerns persist that AI may replace human jobs or diminish the interpersonal nature of care, potentially slowing its widespread adoption (Hofweber & Walker, 2024). Beyond trust, education and training are essential. Healthcare professionals require specialized instruction to use AI tools safely and effectively. Clear guidance on AI’s capabilities and limitations ensures that both healthcare providers and patients remain fully informed about its risks and benefits. AI should be viewed as a complementary tool that enhances, rather than replaces, human clinical judgment. Workforce displacement remains a particular concern, especially for non-professional pharmacists. While fears that AI could lead to job losses are common; however, when properly planned, AI can actually empower pharmacists by expanding their competencies and allowing them to focus on more complex, patient-centered tasks. Instead of reducing the workforce, AI presents opportunities for professional growth and transformation (Sengupta et al., 2024).
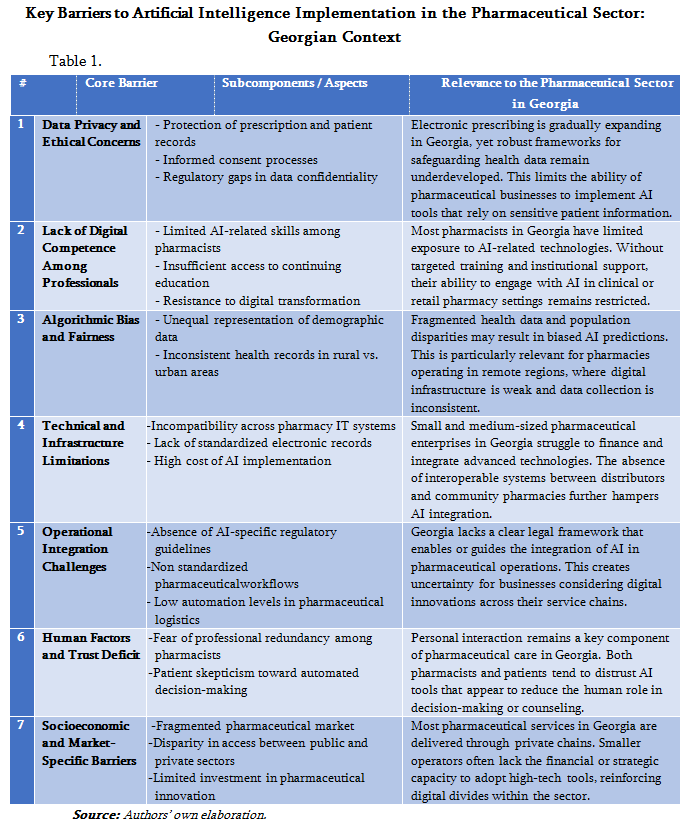
11. To better understand the complex barriers hindering the implementation of artificial intelligence in the pharmaceutical sector, an analytical framework was developed by thematically categorizing the most significant challenges. Considering the unique characteristics of Georgia’s healthcare and pharmaceutical systems – such as underdeveloped digital infrastructure, a fragmented pharmaceutical market, and the slow pace of regulatory adaptation – seven core obstacles were identified. These include data protection and privacy concerns, limited digital literacy, algorithmic bias, technical limitations, difficulties in workflow integration, lack of public and professional trust, and existing socioeconomic inequalities.
These barriers not only reflect global challenges but also highlight the context-specific constraints faced by pharmaceutical professionals and institutions in Georgia. For example, the absence of standardized electronic records and poor interoperability among stakeholders in the pharmaceutical supply chain pose substantial hurdles to AI adoption. Additionally, the cautious attitudes of pharmacists and patients toward AI-driven decision-making underscore the need for targeted education and awareness programs tailored to the local cultural and professional environment.
Table 1 presents a synthesis of the findings, highlighting the seven primary barriers along their specific subcomponents and relevance to the pharmaceutical sector in Georgia. This framework is designed to facilitate the development of context-sensitive policy recommendations and practical implementation strategies.
Discussion
Overcoming Barriers to the Integration of Artificial Intelligence (AI) in Pharmaceutical Practice in Georgia
The potential of artificial intelligence to enhance the pharmaceutical practice in Georgia is undeniable. However, its successful integration faces several challenges, particularly in the areas of technology, education, regulation, and infrastructure. Overcoming these barriers requires a cohesive, strategic approach, fostering collaboration across all levels of the healthcare system (Adler-Milstein et al., 2022).
A key factor in facilitating AI adoption is the modernization of pharmacy education in Georgia. Integrating AI fundamentals into educational programs will ensure that healthcare professionals are adequately trained to use AI technologies ethically and effectively in clinical settings (Bryan & Li, 2024). This will cultivate a workforce capable of embracing and driving digital transformation in the pharmaceutical field. Equally important is collaboration among pharmacists, patients, regulators, and technology developers. Strengthening trust and transparency through coordinated efforts will not accelerate AI adoption but also improve public perception, ultimately driving innovation in healthcare delivery (Sengupta et al., 2024).
Significant investment in research and development is essential to drive AI innovation within Georgia’s pharmaceutical sector. Strengthening national research infrastructure through public-private partnerships can help develop locally relevant AI technologies that are competitive on the global stage (Agarwal & Gao, 2024). Equally important are robust data protection and privacy protocols, ensuring AI applications –often reliant on personal health data – maintain public trust (Adler-Milstein et al., 2022).
AI holds tremendous potential to enhance pharmaceutical care by promoting rational drug use, personalizing treatment plans, and optimizing pharmaceutical services. These capabilities are especially valuable in Georgia, where improving healthcare efficiency is a national priority. However, some pharmacists still view AI as a potential threat to their professional roles. It is essential to clarify that AI is a supportive tool designed to complement, not replace, human expertise (Bryan & Li, 2024). Fostering a better understanding of AI’s role will help mitigate such concerns.
Additionally, addressing technical and financial limitations is crucial for the successful integration of AI. Implementing AI systems requires substantial investments in infrastructure, software, and workforce training. Public-private partnerships can provide sustained support, particularly for smaller pharmacies in regional areas, helping them overcome resource constraints. Public awareness campaigns will also be instrumental in educating stakeholders about AI’s benefits and limitations, ensuring informed decision-making and strengthening trust in the technology (Adler-Milstein et al., 2022).
As Georgia continues to align with international standards, harmonizing its regulatory framework for AI in healthcare with global guidelines is essential to ensure AI interoperability across jurisdictions (Sengupta et al., 2024). Additionally, fostering interdisciplinary collaboration among pharmacists, physicians, data scientists, and engineers will be instrumental in effectively integrating AI into pharmaceutical practice. Platforms that facilitate promote such collaboration will drive innovation and knowledge-sharing, leading to a broader advancement in healthcare (Bryan & Li, 2024).
A critical factor in AI adoption in Georgia is the standardization of health data systems. Given the fragmented nature of Georgia’s digital health infrastructure, achieving seamless interoperability with AI tools presents a challenge. Streamlining and standardizing health data systems is crucial for enabling data-driven decision-making. Furthermore, continuous professional development and ethics-based training programs for pharmacists will help ensure they are equipped to responsibly implement AI applications in their practice (Agarwal & Gao, 2024).
Transparency and accountability in AI systems are fundamental for building trust among healthcare professionals and patients. Establishing mechanisms that explain AI decision-making processes and audit its operations will be critical for fostering confidence in AI solutions (Hofweber & Walker, 2024). Addressing algorithmic biases through training AI models on diverse, inclusive datasets will also ensure equitable healthcare delivery for all patients, regardless of demographic background. Close collaboration with national regulatory bodies will be essential to ensure that AI systems in pharmacy meet both local and international standards (Adler-Milstein et al., 2022).
By addressing these barriers and making strategic investments, Georgia can enhance the efficiency, accessibility, and overall quality of pharmaceutical care through AI integration.
Recommendations for Integrating AI into Georgia’s Pharmaceutical Sector
For the successful adoption of artificial intelligence in Georgia's pharmaceutical sector, a multi-faceted approach is essential. This strategy must go beyond technological advancements to include systematic reforms in education, policy, and public awareness. The following recommendations outline key steps for effective AI integration:
Educational Reforms: To ensure AI is successfully incorporated into Georgia’s pharmaceutical industry, pharmacy education at both undergraduate and postgraduate levels must evolve to include AI-related content. Future pharmacy professionals are equipped with the necessary skills to work efficiently with AI systems. Curricula should cover both technical aspects such as machine learning, data analytics, and algorithm design – and ethical considerations related to AI use. By embedding AI education into academic programs, Georgia can develop a workforce capable of driving digital transformation in healthcare.
Awareness for Pharmacists and Patients: Raising awareness about AI among pharmacists and patients is vital for the smooth implementation of these technologies in pharmacy practice. Pharmacists must understand AI’s capabilities, limitations, data privacy implications, and ethical concerns in patient care. Simultaneously, public outreach campaigns should educate patients on how AI can enhance their healthcare experience while safeguarding their privacy. Transparent communication and open engagement will foster trust in AI technologies, alleviating fears and promoting collaboration between pharmacists, patients, and technology providers.
Public-Private Collaborations: Integrating AI into Georgia’s pharmaceutical practice requires substantial financial investment, particularly for smaller pharmacies in rural areas with limited resources. Establishing public-private partnerships can provide essential financial support and infrastructure for AI adoption. Collaboration among the government, private companies, and academic institutions can create sustainable models for AI integration, ensuring accessibility across all healthcare providers. These partnerships could offer incentives such as funding, training programs, and technology access to promote equitable AI deployment across the country.
Continuous Evaluation of AI Systems: Ongoing monitoring and evaluation are crucial to maintaining the effectiveness and reliability of AI systems in pharmaceutical practice. A robust feedback mechanism should be developed to assess AI performance, identify potential issues, and implement necessary improvements. Regular audits and system updates will address concerns related to accuracy, security, and regulatory compliance. This continuous assessment will ensure that AI tools evolve alongside healthcare needs, optimizing their benefits for both patients and healthcare professionals.
Engaging the Public: Involving the public in the planning and evaluation of AI technologies is vital to ensuring these systems meet societal needs. Public consultations provide an opportunity to gather diverse perspectives on the application of AI in pharmaceutical practice, helping align technological advancements with patient interests and ethical standards. These consultations also uncover concerns that healthcare professionals or developers might not immediately recognize. By fostering broader community involvement, transparency is enhanced, and a shared sense of ownership and trust in AI systems is cultivated.
Establishing Ethical Guidelines: The responsible development and use of AI in pharmaceutical services require clear ethical frameworks that safeguard patients rights, ensure data privacy and address the broader ethical implications of AI in healthcare. These guidelines must prioritize patient well-being and autonomy, ensuring AI-driven systems operate with fairness, transparency, and accountability. Additionally, safeguards should be implemented to mitigate algorithmic biases, guaranteeing equitable care to all patients, regardless of demographic factors.
Successfully integrating AI into Georgia’s pharmaceutical sector demands a comprehensive strategy that address technological advancements, educational initiatives, regulatory alignment, and ethical considerations. By adhering to these recommendations, Georgia can cultivate a healthcare environment where AI enhances the quality, accessibility, and efficiency of pharmaceutical services for both professionals and patients.
The chart presented in Figure N1 illustrates the AI integration process within the pharmaceutical sector, outlining a systematicapproach that includes strategy formulation, needs analysis and risk assessment, regulatory harmonization, modernization of education, infrastructure readiness, pilot projects, public engagement, and, ultimately, the widespread adoption of AI-driven systems
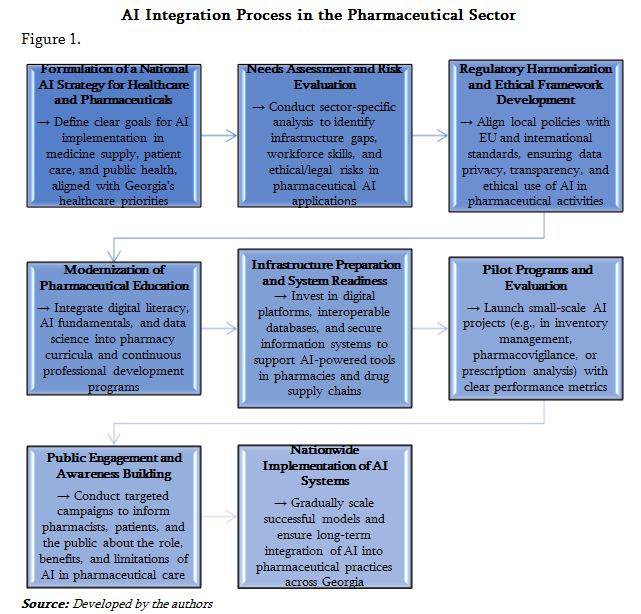
The successful integration of AI technologies into Georgia's pharmaceutical sector demands a multi-faceted approach, progressing through several key stages. From strategic formulation to widespread adoption, each phase is designed to create an environment that fully harnesses modern technology. Moreover, it is vital to consider account for Georgia's current realities, such as infrastructure readiness and professional education – at every stage of implementation. Consequently, careful preparation and sustained long-term investment are essential to ensuring that AI adoption is both effective and purposeful.
Conclusion
The integration of artificial intelligence into Georgia's pharmaceutical practice presents a transformative opportunity to enhance healthcare delivery and medication management. However, these benefits can only be fully realized if legal, ethical, and institutional frameworks evolve alongside technological advancements. This requires investing human capital, fostering interdisciplinary collaboration, and ensuring sustained long-term investment. Through coordinated efforts across all sectors, Georgia can strategically leverage AI to improve the efficiency, accessibility, and quality of pharmaceutical care in a manner that is both an ethical and sustainable.
References::
• Abd-alrazaq, A., Alajlani, M., Alhuwail, D., Househ, M., & Shah, Z. (2022). Artificial intelligence in pharmacy practice: A scoping review. Pharmacy, 10(2), 43. https://doi.org/10.3390/pharmacy10020043
• Adler-Milstein, J., Aggarwal, N., Ahmed, M., Castner, J., Evans, B., Gonzalez, C. A., James, S., Lin, S., Mandl, K., Matheny, M., Sendak, M., Shachar, C., & Williams, A. (2022). Meeting the moment: Addressing barriers and facilitating clinical adoption of artificial intelligence in medical diagnosis. NAM Perspectives. Discussion Paper. https://doi.org/10.31478/202209c
• Agarwal, R., & Gao, G. (2024). Toward an “equitable” assimilation of artificial intelligence and machine learning into our healthcare system. North Carolina Medical Journal, 85(4), 246–250. https://doi.org/10.18043/001c.120561
• Amosu Olamide & Kumar Praveen & Ogunsuji Yewande & Oni Segun & Faworaja Oladapo. (2024). AI-driven demand forecasting: Enhancing inventory management and customer satisfaction. World Journal of Advanced Research and Reviews. 23. 708-719. 10.30574/wjarr.2024.23.2.2394.
• Bryan, J., & Li, D. (2024). Comments on contemporary uses of machine learning for electronic health records. North Carolina Medical Journal, 85(4), 263–265. https://doi.org/10.18043/001c.120561
• Hofweber, T., & Walker, R. L. (2024). Machine learning in healthcare: Ethical considerations tied to privacy, interpretability, and bias. North Carolina Medical Journal, 85(4), 240–245. https://doi.org/10.18043/001c.120561
• Kampanart Huanbutta, Kanokporn Burapapadh, Pakorn Kraisit, Pornsak Sriamornsak, Thittaporn Ganokratanaa, Kittipat Suwanpitak, Tanikan Sangnim, Artificial intelligence-driven pharmaceutical industry: A paradigm shift in drug discovery, formulation development, manufacturing, quality control, and post-market surveillance, European Journal of Pharmaceutical Sciences, Volume 203, 2024, 106938, ISSN 0928-0987, https://doi.org/10.1016/j.ejps.2024.106938.Topol, E. (2019). Deep medicine: How artificial intelligence can make healthcare human again. Basic Books.
• Mosley, Y., Tardif-Douglin, M., & Edmondson, L. (2024). A compass for North Carolina health care workers navigating the adoption of artificial intelligence. North Carolina Medical Journal, 85(4).
• Noorbakhsh-Sabet N, Zand R, Zhang Y, Abedi V. Artificial Intelligence Transforms the Future of Health Care. Am J Med. 2019 Jul;132(7):795-801. doi: 10.1016/j.amjmed.2019.01.017. Epub 2019 Jan 31. PMID: 30710543; PMCID: PMC6669105.
• Norori N, Hu Q, Aellen FM, Faraci FD, Tzovara A. Addressing bias in big data and AI for health care: A call for open science. Patterns (N Y). 2021 Oct 8;2(10):100347. doi: 10.1016/j.patter.2021.100347. PMID: 34693373; PMCID: PMC8515002.
• Riad, M., Naimi, M., & Okar, C. (2024). Enhancing Supply Chain Resilience Through Artificial Intelligence: Developing a Comprehensive Conceptual Framework for AI Implementation and Supply Chain Optimization. Logistics, 8(4), 111. https://doi.org/10.3390/logistics8040111
• Saha Aritra, Singh Indu, Harnessing the Power of Artificial Intelligence in Pharmaceuticals: Current Trends and Future Prospects, Intelligent Pharmacy, 2025, ISSN 2949-866X, https://doi.org/10.1016/j.ipha.2024.12.001.Kumar, A., Thakur, R., & Rana, S. (2022). Pharmacovigilance and artificial intelligence: Opportunities and challenges. Journal of Drug Safety and Health, 8(3), 101–110. https://doi.org/10.1016/j.sapharm.2021.04.002
• Sengupta S, Rao R, Kaufman Z, et al. A health care clinical data platform for rapid deployment of artificial intelligence and machine learning algorithms for cancer care and oncology clinical trials. N C Med J. 2024;85(4):270-273.
• Sharma, A., & Verma, R. (2023). Inventory optimization using artificial intelligence in the pharmaceutical industry. Operations Research Perspectives, 10, 100266. https://doi.org/10.1016/j.orp.2023.100266
• Shashiashvili, N. (2025). Artificial Intelligence in Pharmaceutical Services and the Concept of Pharmaco-Intelligence. Georgian Scientists, 7(2), 69-79. https://doi.org/10.52340/gs.2025.07.02.07
• Wang, Yichuan & Kung, Leeann & Byrd, Terry. (2018). Big data analytics: Understanding its capabilities and potential benefits for healthcare organizations. Technological Forecasting and Social Change. 126. 3-13. 10.1016/j.techfore.2015.12.019.
• Wiljer D, Hakim Z. Developing an Artificial Intelligence-Enabled Health Care Practice: Rewiring Health Care Professions for Better Care. J Med Imaging Radiat Sci. 2019 Dec;50(4 Suppl 2):S8-S14. doi: 10.1016/j.jmir.2019.09.010. Epub 2019 Nov 29. PMID: 31791914.
• Zhang,H. (2023). Artificial intelligence in healthcare: Opportunities and challenges. Theoretical and Natural Science,21,130-134.









